More people are seeking out mental health care, but psychiatrists are in short supply: 'It's getting worse'
| Chicago Tribune |
Mar 24, 2018 | 6:00 AM
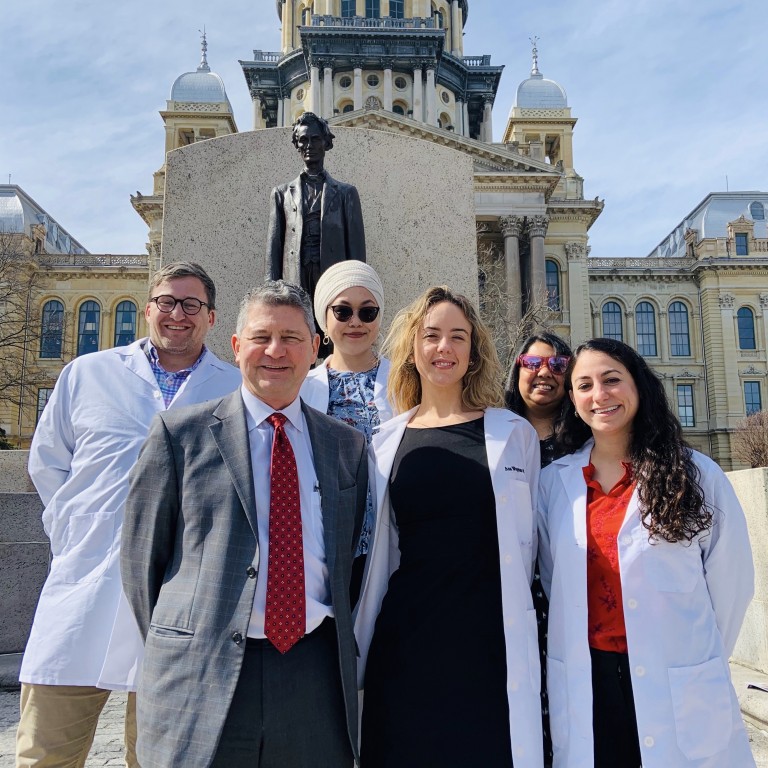
As University of Chicago medical students celebrate Match Day, which is the day they find out where they will do their residencies, Dr. Michael Marcangelo, the school’s director of medical student education in psychiatry, explains why more students are choosing to pursue psychiatry as a specialty, a trend that comes as the nation grapples with a psychiatrist shortage.
Medical student Mila Grossman had just begun her first clinical rotation when she started to get an idea of what kind of doctor she wanted to be.
Working at a women’s mental health clinic, she met a new mom who appeared put-together but inwardly suffered from painful postpartum depression.
Grossman decided to pursue psychiatry and is among a growing share of medical students doing the same.
“That opened my eyes to the severity and stigma that really exist,” said Grossman, 29, who is set to graduate this year from the University of Chicago’s Pritzker School of Medicine and enter a psychiatry residency. “I pretty quickly became intrigued by the patients and fascinated by the transformative effects of therapy and psychopharmacology.”
Psychiatry’s growing popularity as a career choice comes as the nation grapples with a stubborn shortage of psychiatrists that some fear will continue to deepen.
The shortage is most acute in rural areas and poor urban neighborhoods that often aren’t the first choice for in-demand doctors with plentiful options, but is also being felt across big cities as the need for mental health professionals outpaces supply.
[Most read] Lots of rides but broken rules: Chicago’s scooter pilot gets off to a rough start »
“We feel it is an emergency,” said Marvin Lindsey, CEO of the Community Behavioral Healthcare Association of Illinois, which represents mental health agencies that serve mostly low-income residents. "We feel it's getting worse."
We feel it is an emergency. We feel it's getting worse.
Marvin Lindsey, CEO of the Community Behavioral Healthcare Association of Illinois
Share quote & link
The reasons for the shortfall are varied. Greater awareness, diminished stigma, and a worsening opioid crisis are driving more people to seek mental and behavioral health care. Meanwhile, nearly 60 percent of psychiatrists are over age 55, fueling a retirement wave that experts say exceeds the pipeline of new doctors who fill limited psychiatric residency slots.
Low insurance reimbursement rates for psychiatrists might also be keeping some people from pursuing the specialty, or, if they do, from joining insurance networks, which keeps services out of reach of many people who can't afford to pay out of pocket.
An additional challenge is that procedure-oriented doctors often prefer the more straightforward payoff of mending a broken arm or repairing a damaged heart.
“There’s no victory lap (in psychiatry) where you can say you fixed that patient, on to the next one,” said Travis Singleton, senior vice president of physician staffing firm Merritt Hawkins. “It is lifetime management.”
[Most read] Column: That waitress who spit on Eric Trump? She’s lucky I’m not king. »
The shortage of psychiatrists, who are distinct from psychologists and other general mental health service providers because they can prescribe medication, is not evenly spread. Chicago has plenty of private psychiatric practices, and some residential facilities say they are well-staffed thanks to being able to offer good salaries and the work arrangements doctors request.
But community health clinics and some low-income hospitals struggle to hire psychiatrists, which limits their ability to provide services and forces more mental health cases into emergency rooms not staffed to deal with them. While the number of medical students pursuing psychiatry is growing, it’s not enough — and they don’t necessarily end up practicing where the need is greatest.
Staffing challenges
The Chicago Department of Public Health has felt the pinch as it tries to staff its five community mental health clinics, said spokeswoman Erica Duncan. It increased starting salaries for psychiatrists, to $109 an hour from $87.76 in 2015, redoubled its recruitment efforts and was approved as a health shortage site so its psychiatrists can qualify for a federal school loan repayment program that rewards doctors who treat underserved populations.
But “even with these added incentives, we continue to face challenges in recruiting and hiring permanent staff,” Duncan said in an email. This spring the department will start offering telepsychiatry, connecting patients to psychiatrists via video conference, to ease the crunch.
At St. Bernard Hospital in Chicago’s Englewood neighborhood, CEO Charles Holland said it has been extremely difficult to recruit psychiatrists as it expands its mental health services.
In response to growing need — driven in part by more patients with drug-induced psychosis landing in the emergency room — the hospital three years ago opened an outpatient mental health clinic and next month will expand its inpatient mental health unit to 60 beds from 40.
But the hospital, which serves a primarily low-income population on Medicaid, has found that many young psychiatrists with medical school debt choose to work at more affluent hospitals that can afford better pay, or at academic centers where they can spend part of their time on research, said Chief Operations Officer Roland Abellera.
St. Bernard considered hiring a staffing agency to help but can’t afford the $30,000-per-doctor finder’s fee, Abellera said. The hospital is instead moving toward using more nurse practitioners to prescribe medication and plans to offer telepsychiatry, he said.
Doctors say insufficient psychiatric services in the community have driven more mental health issues into emergency rooms, where psychiatric patients increased 42 percent between 2014 and 2017.
At Presence Resurrection Medical Center on Chicago’s Northwest Side, many such patients arrive late at night, after the clinical crisis workers have gone home, causing long delays in their transfer to an appropriate facility because the evaluation has to wait until morning, said Dr. David Bordo, regional medical officer.
“It’s probably the worst place to spend the night because of all the stimuli,” he said.
[Most read] From sacred to secular: What happens when a Catholic church shuts down? »
In October the hospital launched a telecrisis pilot program that connects those patients, via tablet, to a crisis worker staffing the overnight shift at another facility, to get the transfer paperwork started. It used the system more than 70 times during the last three months of 2017, Bordo said.
Central DuPage Hospital, which recently expanded its substance abuse unit in response to rising opioid-related visits, started a pilot telepsychiatry program last April to cover weekend shifts, said Allison Johnsen, manager of business and program development at the hospital. It has two of its psychiatrists patch in from home to conduct consultations via a tablet brought to patients’ bedsides.
The program, which Johnsen says has been well-received by patients, helps with recruitment because it offers doctors flexibility and lightens their load.
“Physicians coming out of medical school are looking for more work-life balance,” Johnsen said.
Pipeline of doctors
Meanwhile, the supply of new psychiatrists is growing.
The number of U.S. medical students matching into psychiatry residencies rose to 982 this year, representing 5.5 percent of all matches, up from 681 students, or 4.2 percent of all matches, five years ago.
Dr. Daniel Yohanna, interim chair of the University of Chicago’s Department of Psychiatry, attributes the growing interest in part to more scientific evidence of psychiatry’s effectiveness.
“It reduces the stigma around psychiatry, both for students and our colleagues in other areas," Yohanna said.
At University of Chicago’s medical school, 10 students in the 2018 graduating class are pursuing psychiatry, a record for the school, which typically sees five or six, said Dr. Michael Marcangelo, the school’s director of medical student education in psychiatry.
The most important reason for the rise, Marcangelo said, is that “psychiatry is the last field of medicine that really pays a lot of attention to people as people.”
“The rest of medicine is becoming very technical,” he said. “A lot of people who go into medicine want to work closely with patients.”
Grossman, the student whose experience at the women’s mental health clinic helped shape her interest in psychiatry, said psychiatry is “not necessarily what you think of when you enter medical school.” But she soon discovered that she was drawn to learning about the psychosocial aspects of patients’ cases.

Mila Grossman, 29, of the University of Chicago's Pritzker School of Medicine, opens her letter with her fiance, Rohan Agarwal, at a Match Day event on the University of Chicago campus in Chicago on March 16, 2018. (Jose M. Osorio / Chicago Tribune)
Earlier this month on Match Day — the day all U.S. medical school students find out where they will do their post-graduation residencies — Grossman sat among her classmates in a crowded lecture hall, her finger poised at the edge of her acceptance envelope and ready to rip when the countdown was done. The letter inside revealed she had matched into her first-choice psychiatry residency, at Massachusetts General Hospital, sparking big hugs and high-fives all around.
Grossman hopes to specialize in treating women managing mental illness during and after pregnancy, ideally in an academic medical center so she can also do research and teach.
Addressing the shortage
While interest in psychiatry grows, demand is growing faster. For two consecutive years, psychiatry has been the second-most requested search assignment at staffing firm Merritt Hawkins, after family medicine, and is the most difficult specialty to fill, Singleton said. A decade ago, psychiatry was ninth on the list.
Where and what psychiatrists end up practicing after their four-year residency ends matters most in addressing the shortage, said Dr. Sidney Weissman, clinical professor of psychiatry and behavioral sciences at Northwestern University’s Feinberg School of Medicine. Many decide it is in their financial interest to go directly into private practice rather than continue collecting a resident stipend for a fifth year as they train in a subspecialty where the need is most dire, such as geriatric or child and adolescent psychiatry, Weissman said. He advocates letting psychiatrists train in a subspecialty in their fourth year of residency to make it more economically viable.
“Psychiatry has to look at itself to rethink how we do business,” Weissman said. “It needs to relook at how we train people, how long is the training and what we expect them to do.”
Concerns about a psychiatrist shortage often point to compensation, which, though handsome and rising, is less than many other specialties. Starting annual salaries for psychiatrists range from $239,000 to $272,000, compared with a range of $429,000 to $529,000 for radiologists and more than $600,000 for orthopedic surgeons, according to Merritt Hawkins. Internal medicine, pediatrics and family practice also pay on the lower end and face doctor shortages.
Psychiatric services also are reimbursed by insurance at lower rates than other medical procedures, which could be why about 40 percent of psychiatrists practice in cash-only private practices, according to the National Council Medical Director Institute.
Medicaid rates are particularly low, which makes it tough to get psychiatrists to work with high-Medicaid populations, Lindsey said.
Community clinics historically have relied on other funding to round out psychiatrist incomes and say state funding cuts have hurt those efforts. Illinois’ proposed 2019 budget allocates $47 million less for mental health than it did the prior year, according to the Illinois Association for Behavioral Health.
The crunch is forcing some providers to rethink how they provide services.
Turning Point, an outpatient mental health center in Skokie, had received a private foundation grant to hire a part-time advanced practice psychiatric nurse — a position that can prescribe medication — but abandoned the search after repeated recruitment efforts failed.
“The demand for people with those credentials is so huge, and when we had interviews it was a matter of them having other options,” said CEO Ann Raney. It remains a sorely needed position at the center, where about half of the 1,300 people it serves annually take medication, she said.
Turning Point renegotiated the terms of the grant and instead used it on administrative support for the existing psychiatric staff members, so they can spend less time on paperwork and more seeing patients, Raney said. The facility also is limiting psychiatric services to only patients who prove their commitment to therapy, because it doesn’t have the staffing to handle more.
“That’s the tragedy,” Raney said. “We could do so much more if we had more people.”
Cook County Jail had to scramble when it lost 11 of its 15 psychiatrists in 2011, after a federal program that provides student loan assistance to physicians who work in underserved areas removed all county and municipal correctional facilities from its approved site list.
It has since replenished its psychiatric staff by boosting salary offers and talking up the perks of working at a jail, such as the administrative staff that takes care of the billing process so psychiatrists can focus on the patient, said Dr. Claudia Fegan, chief medical officer at Cook County Health and Hospitals System, which operates the jail’s health services.
Legislation to address the state’s psychiatrist shortage is in the pipeline.
A bill introduced in the Illinois House in February aims to lift Medicaid reimbursement rates for psychiatric treatment by tying them to higher Medicare rates. Another calls for creating a Behavioral Health Education Center, administered by a state university, with psychiatry residency slots plus internships for other mental health professionals who would be placed in underserved communities.
Meanwhile, a state law passed in 2014 allows licensed clinical psychologists with advanced, specialized training to prescribe certain medications to treat mental health disorders. About 150 psychologists are undergoing the extensive training required to apply, many of them in hospitals in central and southern Illinois where they will stay and practice said Beth Rom-Rymer, who led the movement to pass and implement the legislation when she was president of the Illinois Psychological Association.
“There is tremendous interest,” Rom-Rymer said. “Psychologists are very enthusiastic about being able to gain these skills and broaden their authority.”
aelejalderuiz@chicagotribune.com
Twitter @alexiaer
- Medical Research
- Hospitals and Clinics
- Mental Health Research
- Mental Health
- Drugs and Medicines
- Medicaid
- University of Chicago
Alexia Elejalde-Ruiz
Alexia Elejalde-Ruiz covers the food industry for the Chicago Tribune's business section. Prior beats include workplace issues, the retail sector, and lifestyle features, plus stints at RedEye, the Daily Herald and the City News Service. Alexia grew up in Washington, D.C., and has her degree in international relations from Brown University.
Advertisement