https://www.the-scientist.com/features/how-social-isolation-affects-the-brain-67701
Absence of human contact is associated with declines in cognitive function. But as the COVID-19 pandemic brings concerns about the potential harms of isolation to the fore, researchers are still hunting for concrete evidence of a causal role as well as possible mechanisms.
Jul 13, 2020
Daisy Fancourt was at her home in Surrey in southeast England when the UK government formally announced a nationwide lockdown. Speaking in a televised address on March 23, UK Prime Minister Boris Johnson laid out a suite of measures designed to curb the spread of COVID-19, including closing public spaces and requiring people to stay home except for exercise and essential tasks. For Fancourt, an epidemiologist at University College London (UCL), the announcement meant more than just a change to her daily life. It was the starting gun for a huge study, weeks in the planning, that would investigate the effects of enforced isolation and other pandemic-associated changes on the British public.
We’re a social species. We really need others to survive.
—Stephanie Cacioppo,PhD University of Chicago
In more normal times, Fancourt and her colleagues study how social factors such as isolation influence mental and physical health. Before Johnson’s late-March announcement, the team had been watching as Italy, and subsequently other countries in Europe, began closing down public spaces and enforcing restrictions on people’s movements. They realized it wouldn’t be long before the UK followed suit. “We felt we had to start immediately collecting data,” Fancourt says. She and her colleagues rapidly laid the groundwork for a study that would track some of the effects of lockdown in real time. Between March 24 and the middle of June, the study had recruited more than 70,000 participants to fill out weekly online surveys, and in some cases answer questions in telephone interviews, about wellbeing, mental health, and coping strategies.
This project and others like it underway in Australia, the United States, and elsewhere aim to complement a broader literature on how changes in people’s interactions with those around them influence their biology. Even before COVID-19 began its global spread, millions of people were already what researchers consider to be socially isolated—separated from society, with few personal relationships and little communication with the outside world. According to European Union statistics, more than 7 percent of residents say they meet up with friends or relatives less than once a year. Surveys in the UK, meanwhile, show that half a million people over the age of 60 usually spend every day alone.

© ISTOCK.COM, MARIA ZAMCHY
These figures are concerning to public health experts, because scientific research has revealed a link between social isolation—along with negative emotions such as loneliness that often accompany it—and poor health. “We are seeing a really growing body of evidence,” says Fancourt, “that’s showing how isolation and loneliness are linked in with incidence of different types of disease [and] with premature mortality.” Alongside myriad connections to poor physical health, including obesity and cardiovascular problems, a range of possible effects on the human brain have now been documented: Social isolation is associated with increased risk of cognitive decline and dementia, as well as mental health consequences such as depression and anxiety.
It’ll be years before researchers understand whether and how measures enacted during the pandemic play into any of these risks. The sort of isolation people are experiencing right now is unprecedented, and is compounded with other pressures, such as fear of disease and financial strain. But now more than ever, it’s important to study the effects of social isolation, and potential means to mitigate it, says Stephanie Cacioppo, a social neuroscientist and cognitive psychologist at the University of Chicago. “We’re a social species,” she says. “We really need others to survive.”
The cognitive effects of prolonged social isolation
In 1972, French adventurer and scientist Michel Siffre famously shut himself in a cave in Texas for more than six months—what still clocks in as one of the longest self-isolation experiments in history. Meticulously documenting the effects on his mind over those 205 days, Siffre wrote that he could “barely string thoughts” together after a couple months. By the five-month mark, he was reportedly so desperate for company that he tried (unsuccessfully) to befriend a mouse.
This kind of experiment, and less extreme isolation periods such as those experienced by spaceship crews or scientists working in remote Antarctic research stations, has offered glimpses of some of the cognitive and mental effects of sensory and social deprivation. People routinely report confusion, changes in personality, and episodes of anxiety and depression. A crueler version of those experiments is continually underway in prisons across the world. In the US alone, tens of thousands of incarcerated people are in long-term solitary confinement, with devastating and lasting effects on cognitive and mental health. (See “Extreme Isolation” below.)
For most of human society, however, social isolation acts in more insidious ways than these “experiments” capture, often disproportionately affecting vulnerable members of the population, such as the elderly, and with effects accumulating slowly such that they may go unnoticed for many years, if not decades. The effects of this subtler sort of social isolation, which some health researchers and psychologists have already described as a public health risk, are better observed in longer-term studies that look for links between a person’s social connections and how the mind functions.
Many studies have found that chronic social isolation is indeed associated with cognitive decline, and that isolation often precedes decline by several years. One 2013 study, for example, measured cognitive function at two time points in a cohort of more than 6,000 older individuals taking part in the English Longitudinal Study of Ageing (ELSA). People who reported having fewer social contacts and activities at the beginning of the study, researchers found, showed greater decline in cognitive function, as measured by verbal fluency and memory recall tasks, after four years.
More-recent studies have added weight to the association. A 2019 study of more than 11,000 people taking part in ELSA found that men who reported higher-than-average social isolation and women who reported increasing social isolation both experienced above-average decline in memory function within two years of being surveyed. However, the results don’t demonstrate that isolation causes deterioration in brain function, cautions ELSA director Andrew Steptoe, a UCL psychologist and epidemiologist who collaborates with Fancourt; it’s also possible that cognitive decline encourages some people to socialize less.
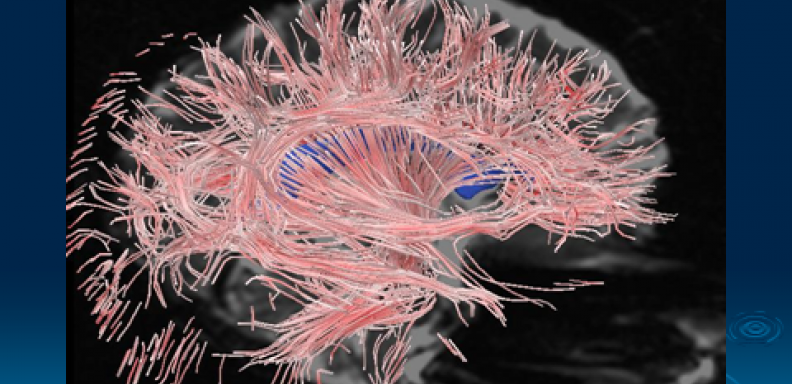
THE ISOLATED BRAINStudies of animals and people experiencing isolation have identified several brain structures that appear to be affected by a lack of social interaction. Although these studies can’t identify causal relationships—and don’t always agree with one another—they shine a light on some of the mechanisms by which physical isolation, or feelings of loneliness, could impair brain function and cognition.
© ISTOCK.COM, JAMBOJAM PREFRONTAL CORTEX: In some studies, people who are lonely have been found to have reduced brain volumes in the prefrontal cortex, a region important in decision making and social behavior, although other research suggests this relationship might be mediated by personality factors. Rodents that have been isolated from their conspecifics show dysregulated signaling in the prefrontal cortex. HIPPOCAMPUS: People and other animals experiencing isolation may have smaller-than-normal hippocampi and reduced concentrations of brain-derived neurotrophic factor (BDNF), both features associated with impaired learning and memory. Some studies indicate that levels of the stress hormone cortisol, which affects and is regulated by the hippocampus, are higher in isolated animals. AMYGDALA: About a decade ago, researchers found a correlation between the size of a person’s social network and the volume of their amygdala, two almond-shaped brain areas associated with processing emotion. More-recent evidence suggests the amygdalae are smaller in people who are lonely. |
See full infographic: WEB | PDF
Indeed, the relationship between isolation and cognitive health isn’t entirely clear-cut. A recent meta-analysis of more than 50 studies, carried out by clinical psychologist Linda Clare and colleagues at the University of Exeter, found that while there was reasonably good evidence for an association between social isolation and cognitive decline later in life, the relationship wasn’t as strong as that reported for cognitive decline and some other lifestyle factors such as educational attainment. “We have to acknowledge that there are lots of different measures used and different studies and different ways of approaching this,” says Clare, whose work focuses on ways to help dementia patients and their caregivers in the UK. Different studies assess social isolation and cognition differently, and not all research takes into account potential confounding factors such as isolated people’s frequency of leisure activities, or their participation in voluntary or paid work. Despite all the variability, Clare says, “we did see that there is a reasonably robust association between more engagement in social activity and better cognitive function in later life.”
To add to the challenges in understanding these complex relationships, there’s sometimes confusion in the scientific literature about the distinction between objective and subjective measures of isolation, notes Cacioppo. “We know that there’s a difference between being physically isolated and emotionally isolated,” she says. Not everyone with limited social connections feels lonely, and some people with lots of social connections do. Cacioppo adds that while some people might choose solitude without suffering particularly adverse effects, loneliness is an inherently negative emotion, and when experienced for long periods, is often associated with depressive symptoms. “Loneliness is a discrepancy between what you want and what you have” in your relationships, she says.

© ISTOCK.COM, MARIA ZAMCHY
A number of studies have tried to parse these subtleties by measuring social isolation and loneliness in parallel, partly aided by a metric known as the University of California, Los Angeles (UCLA) loneliness scale. This scale, developed by UCLA researchers in the 1970s, uses a list of statements to evaluate how connected people feel, in contrast to measures of social isolation, which rely on more-objective measures of social network size or the frequency of contacts with other people. One recent longitudinal study in England found that social isolation and loneliness were each associated with poorer physical and mental health, and the strongest association was seen in the group of people who reported both conditions. A three-year study of adults in Spain published in 2019, meanwhile, found that loneliness and social isolation were independently associated with cognitive decline. Other work has found effects for only one of the two measures: Studies in the Netherlands and the UK, for example, have found that loneliness, but not social isolation, was predictive of the onset of dementia. In contrast to these findings, a preprint published on bioRxiv a few months ago reported that social isolation, but not loneliness, was associated with elevated dementia risk among more than 150,000 adults in the UK when genetic risk factors for dementia were taken into account.
“It’s quite a varied picture,” says Steptoe. “One sometimes finds different patterns.”
Possible mechanisms linking isolation to brain function
By the time the nine-person crew of the Antarctic research station Neumayer III emerged from their 14-month stay a couple of years ago, they’d endured winter temperatures of -50 °C, drastic changes in natural light, and prolonged lack of contact with the outside world. The effects on their brains, it turned out, were substantial.
Structural MRI performed by neuroscientists at the Max Planck Institute for Human Development before and after the trip showed anatomical changes to the dentate gyrus, a region of the brain that feeds information into the hippocampus and is associated with learning and memory; the crew members’ dentate gyruses had shrunk by an average of around 7 percent. The crew members also had reduced blood levels of brain-derived neurotrophic factor (BDNF), a protein involved in stress regulation and memory, and they performed worse on tests of spatial awareness and attention than they had before they left.
The participants in this study were contending with more than just social isolation during their expedition, making it hard to know whether the observed brain changes are linked to lack of social contact as opposed to circadian disruption or some other aspect of their experience. But researchers studying social isolation and loneliness in the general population are also beginning to document differences in brain structure that could help reveal biological mechanisms at play. (See illustration above.)
Surveys already suggest that many people have felt increasing loneliness since the pandemic began.
Sandra Düzel, a neurobiologist at the same Max Planck Institute (though not a collaborator on the Antarctic study), recently set out to study such differences in more than 300 people participating in a longitudinal project called the Berlin Aging Study. Using MRI to map the volume of the brain’s various regions, Düzel and her colleagues found that, regardless of their level of social contact, people who scored high on the UCLA loneliness scale tended to have smaller gray matter volumes in a handful of regions. Those areas included the hippocampus and the amygdala, known for its role in emotion processing. The findings don’t demonstrate that loneliness causes shrinkage of these brain structures, Düzel writes in an email to The Scientist, but the researchers are considering both a lack of social stimulation and loneliness-induced stress as possible contributing factors.
Recent research in mice, which, like humans, are social organisms, supports a role for social interaction in maintaining normal brain structure and function, and hints at possible molecular mechanisms. One 2018 study, for example, investigated the effects of social isolation on mice’s ability to recognize other individuals—something researchers assess by recording how long mice spend interacting with one another, as an unfamiliar mouse normally elicits more interest than a familiar one. Adult mice that had been kept in isolation for up to a week were worse at discriminating familiar and unfamiliar mice, the researchers found. Returning mice to enclosures containing their colony mates restored their recognition abilities, as did inhibiting a small signaling protein known as Rac1, which has been linked to memory problems in Alzheimer’s disease. Activating Rac1 in mice that had not been isolated caused the animals to show the same forgetfulness exhibited by isolated individuals.
While distinguishing between loneliness and social isolation is impossible in animal studies, these kind of manipulative experiments offer a unique insight into effects of isolation on the brain, says Moriel Zelikowsky, a neuroscientist at the University of Utah School of Medicine. Mouse work she carried out while a postdoc at Caltech, for example, revealed a previously unknown role for Tac2, a signaling neuropeptide implicated in diverse cognitive functions, in mediating the behavioral effects of isolation.

© ISTOCK.COM, MARIA ZAMCHY
The peptide was highly expressed across broad regions of the brain in mice that had been housed alone for several weeks, the team found, but not in controls kept with two other mice, nor in rodents isolated for just 24 hours. Mice that had spent weeks by themselves also displayed aggression—a typical behavioral effect of isolation—but that behavior was inhibited by a drug that blocks the protein receptor that Tac2 normally binds to. The findings suggest that Tac2 may be involved in regulating some of the effects of long-term isolation, rather than immediate stress induced by separation from companions, Zelikowsky notes. She adds, however, that there’s still a lot about the neuropeptide the team doesn’t know, including how it may interact with hormones involved in the stress response and whether it functions the same way in humans.
One area where animal studies and observational research in humans may be starting to align is the link between isolation and inflammation—a response that can have negative effects on cognitive function as well as on other processes throughout the body. For example, more than a decade of animal work has shown increased circulation of inflammatory signaling molecules such as interleukin-6 in isolated mice, and a recent meta-analysis of more than two dozen human-focused papers on the topic noted that studies of people experiencing loneliness consistently reported increased blood concentrations of this same cytokine. The meta-analysis also found that social isolation was primarily linked to higher levels for C-reactive protein (CRP) and fibrinogen, two molecules involved in inflammatory responses in mice and humans.
Fancourt, a coauthor of one of the studies included in that meta-analysis, says that the picture starting to emerge from this line of research is that social isolation and loneliness have distinct but closely related effects on inflammatory responses. Her study found that social isolation was associated with higher levels of CRP and fibrinogen, while loneliness was associated with lower insulin-like growth factor-1, a molecule that helps inhibit inflammation. “Both isolation and loneliness were linked to inflammation,” she says, “but while social isolation was linked to inflammatory markers themselves, for loneliness it was related to a pathway that involved how much those inflammatory responses are allowed to happen, or are inhibited from happening.”
If we’re all putting in lots of extra effort to speak to people, are we able to offset some of the negative effects of isolation?
—Daisy Fancourt, University College London
Like research on any potential health risk, studies of social isolation still struggle to connect the dots between observations and concrete biological outcomes. Human studies can only reveal correlations, and experimental animal research “can show you that pathways can work in principle, but it doesn’t show they operate like that” in practice, says Steptoe. Nevertheless, research so far has helped to flesh out neuroscientists’ understanding of the sorts of factors involved in responses to social isolation—and, perhaps more importantly, has inspired several efforts to mitigate the problems that such isolation may cause.
Protecting cognition in socially isolated people
In recognition of the potential risks of social isolation, whether they be related to brain health or to other, less direct risks of living alone, many countries and health organizations have funded outreach campaigns to improve connections between people most likely to be (or to feel) isolated and the rest of the community. Cohousing organizations in the US and elsewhere, meanwhile, aim to foster social engagement with shared living spaces, although their ability to reduce loneliness has yet to be evaluated.
Where changes in a person’s social life or living arrangement aren’t possible or are unlikely to improve the situation, some researchers argue that pharmacological treatments could help—at least temporarily. Cacioppo and her late husband John, a pioneer in the study of loneliness and social neuroscience, proposed a few years ago that allopregnanolone, a steroid involved in regulation of BDNF as well as various emotional and behavioral responses to stress, might help alleviate loneliness in humans. Since 2017, Cacioppo’s team has been working with lonely patients to test a closely related molecule, pregnanolone, although the work has had to be put on hold because of the pandemic.

© ISTOCK.COM, MARIA ZAMCHY
Zelikowsky notes that osanetant, the drug that she and her colleagues used to block Tac2 receptors in their mouse experiments, may also have promise as a therapeutic for people experiencing chronic isolation. The drug was originally developed in the 1990s by France-based pharmaceutical company Sanofi-Synthélabo (now Sanofi) as a treatment for schizophrenia, but was discontinued due to lack of efficacy, she says, adding she doesn’t know of clinical work currently underway to investigate its potential for people experiencing isolation or loneliness.
Other researchers, meanwhile, are focusing on behavioral interventions that may help reduce the risk of cognitive decline and other effects associated with social isolation. Fancourt and Steptoe, for example, have shown that boosting cognitive engagement, regardless of a person’s social engagement, may have a protective effect. One recent study found that people who more frequently visited museums, galleries, or exhibitions or attended theater performances, concerts, or operas were less likely to show decreases in memory recall and verbal skills within the next decade. (The relationship didn’t hold for visits to the cinema.) A 2019 study by the same researchers suggests that engaging in these kinds of cultural activities is associated with a lower risk of dementia.
It’s this kind of area in which research from the ongoing pandemic might also really contribute, says Fancourt. During the crisis, millions of people have found themselves isolated without choosing to be that way, and surveys already suggest that many people—particularly women, according to one recent study in the UK—have felt increasing loneliness since the pandemic began.
While some people may appreciate the chance to be alone, others have found new ways to stay connected with their social network—behaviors that could provide critical information about how different people cope with the effects of being physically separated from society. For example, Fancourt says, “if we’re all putting in lots of extra effort to speak to people, have Skype calls, Zoom calls, message people, are we able to offset some of the negative effects of isolation?”
From a research perspective, she adds, it’s an unprecedented opportunity to ask new questions about how a lack of traditional social contact influences human biology. “It might really change the way we think about concepts like loneliness and isolation,” Fancourt says, “and mean that we might actually start to define and research them differently based on what this very unusual natural experiment teaches us.”
Extreme IsolationEvery year in the US, tens of thousands of incarcerated people spend weeks or months at a time alone in small windowless cells, deprived of sensory stimuli and separated from other people. Surveys of people who have experienced this form of extreme isolation point to a range of negative cognitive consequences, including difficulties thinking or remembering information, obsessive thinking, and hallucinations and other psychotic symptoms, as well as longer-term mental illness risks, and increased incidence of suicide. Research on these effects of solitary confinement isn’t new; in the 19th century, observers of incarcerated people began attributing high rates of psychotic illnesses to having been housed alone and deprived of sensory stimulation, while work carried out in the last few decades in countries including Canada, Norway, South Africa, and Switzerland have drawn similar conclusions. Animal studies that try to mimic the conditions of solitary confinement, meanwhile, indicate numerous potential biological effects on the brain. Studies of mice, for example, show that the stress induced by prolonged isolation can cause changes in brain structure, including reduced hippocampal volume, plus changes in the expression of genes associated with neuroplasticity and chemical signaling. Neuroscientists face an uphill battle in using this research in legal settings for people who have experienced solitary confinement. Many US courts have rejected evidence of psychological pain on the grounds that, unlike a diagnosed mental illness or physiological harm, it is insufficient evidence of “cruel and unusual punishment,” and therefore doesn’t count as a violation of the US Constitution. Neurobiological research based on animal studies, meanwhile, has been rejected on the grounds that animal-based studies cannot be extrapolated to humans. That said, a landmark settlement between incarcerated people and the governor of California in 2015 was decided partly on the basis on neuroscientific evidence and resulted in the end of indeterminate solitary confinement in the state’s prisons. |